Molly’s Story
Like many young couples, first time parents Susan and John looked forward to the arrival of their daughter with excitement and anticipation. But after a difficult pregnancy and the threat of miscarriage, they were not prepared for the challenges they’d face when Molly arrived.

Born prematurely at just 27 weeks in July of 2000, Molly’s birth weight was less than 2 pounds. Like many other preemies, she had trouble with the basic instincts that would keep her alive, such as breathing and eating. Her very tiny and fragile body wasn’t ready to support itself, and required intensive care and machines to stay alive.
Over the course of her first several months, Molly improved slowly, hindered by one complication after another. During a surgical procedure to check for an intestinal blockage, Molly stopped breathing on her own. She was having bronchial spasms and had to be put back on a ventilator. After 6 months in the hospital, specialists had no choice but to perform a tracheotomy.
During that procedure, Molly’s airway and connecting tissue disintegrated when the surgeon made the incision. After a few critical moments, the surgeon was able to improvise by inserting an endotracheal tube. Susan and John, who were waiting outside, heard the words no parent ever wants to hear — “prepare for the worst.” Following surgery, Molly was sedated for 3 weeks and was fed by IV. After several setbacks, including a cardiac arrest, Molly was finally stable enough to be transferred to Franciscan Children’s. It was there that she would begin the long road of rehabilitative treatment.
She wasn’t rolling over, sitting up, or eating solid foods.
When she arrived at Franciscan, she was 8 months old, and unable to carry out the developmentally appropriate activities for a baby her age. She wasn’t rolling over, sitting up, or eating solid foods.
Molly’s team developed a rehabilitation plan that would facilitate her improvement, and over the course of the next several months, therapists worked to gradually wean her off the ventilator. Following the Neonatal Abstinence Syndrome Protocol, the team also began weaning Molly from dependency on the medications she had been receiving since birth.
A nutritionist tracked Molly’s nutritional needs and weight gain, ensuring that her feeding tube was delivering the nutrition she needed to support her development and growth. Occupational, Physical, and Speech Therapists worked with her to lay the groundwork for the development of fine motor skills, ambulation, and feeding skills.
During the entire process, the Franciscan Children’s staff involved Susan and John in Molly’s care, teaching them how to do tracheotomy care and the myriad of other tasks she required. Alternating shifts, they stayed at Molly’s bedside for months, participating and marveling at Molly’s steady improvement in mobility and endurance.
At 11 months old, Molly was finally discharged to go home for the very first time. Before their departure, Susan and John participated in a “leave of absence,” which allows parents to manage care of their child with staff not intervening, but available to help in case the need arises. “When the time came, we felt educated and confident in our abilities to care for Molly at home,” said John.
Since then, it’s been a long road. Molly’s had reconstructive surgery at the tracheotomy site. She’s had a cochlear implant to compensate for the hearing loss she experienced from the life-saving medications she was given as an infant. But those obstacles make her successes even sweeter.
“Another hospital may have saved Molly’s life, but Franciscan Children’s gave her a life to live. For that, we are grateful.”
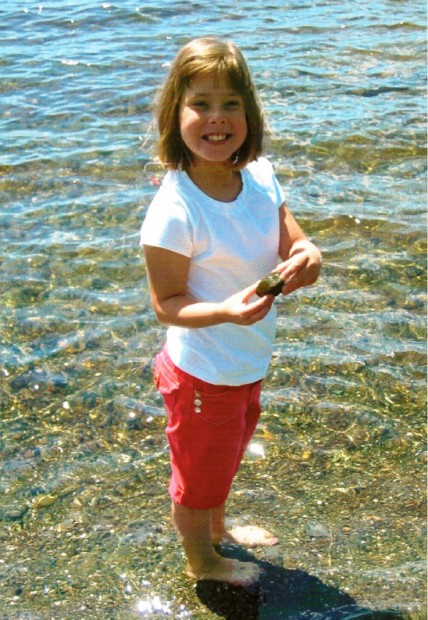
Today, Molly is a second grader in public school who, to her parents’ delight, loves to dance, play softball, and jump rope. One look at her vibrant smile, and it’s impossible to tell how much differently life could have turned out for her. “We could spend our life mourning over Molly’s infanthood, but then we would never be free to enjoy the very special, very lovely things about her just as she is,” said John. “Another hospital may have saved Molly’s life, but Franciscan Children’s gave her a life to live. For that, we are grateful.”
Today, he and Susan are optimistic about all the future holds for Molly.
Want to share your story? Send it our way to stories@fhfc.org.
Explore All Stories